The United Statesissynonymous withaddiction.
In a given year, as many as46.8 million(16.7%) Americans over the age of 12 are diagnosed with a substance use disorder.Doctors have never been busier – or moreaddicted to substances. They are not immune to the deathly grip ofaddiction. Itisestimated that up to15% ofdoctorsare battling with drugand/or alcohol dependency.That means for every sevendoctors, at least one of themisanaddict.
A recent report byAmericanAddiction Centersshines a much-needed light on the many substances usedand abused by physicians. Interestingly, different disciplines are associated with different types of substance abuse.
A recent report by American Addiction Centers shines a much-needed light on the many substances used and abused by physicians. (iStock)
Takeanesthesiologists, for example. Many who areaddicted are typically hooked on potent intravenous opioids like fentanyland sufentanil. These drugs are often taken from the workplace, sometimes from their own patients.
DRUG OVERDOSES HAVE REACHED RECORD HIGH, PER LATEST CDC REPORT: ‘GRIM STATISTICS’
Several factors contribute to the high prevalence of drug abuse amonganesthesiologists, including their close proximity to highlyaddictive substances in the operating room, the ease of diverting these drugs for personal consumption,and the stressful work environment they operate in.
Additionally, according to the report, thereisevidence suggesting that exposure to aerosolized intravenousanesthetics in the workplace can sensitize the brain’s reward pathwaysand lead to subsequent opioid abuse amonganesthesiologists.
Psychiatrists, meanwhile, struggle with benzodiazepine abuse. Surgeons, particularly female surgeons, turn to alcohol for support. As the report notes, 25.6% of female surgeons experience alcohol abuse or dependenceissues, in contrast to 13.9% of male surgeons. These rates significantly surpass the6% prevalenceof alcohol use disorder among the general adult population in the United States.
Emergency medicine physicians, despite making up only 3% of all physicians, constitute a significant portion of physicians enrolled in Physician Health Programs for substance abuse management, ranging from 7-18%. In comparison to other specialties, emergency medicine physicians were found to have a higher prevalence of illicit drug use, particularly cannabis use, according toanother study.
Given their position at the forefront of providing care, emergency medicine physicians constantly face demandingand unpredictable situations. Consequently, their professionisassociated with high levels of stress. In fact, emergency medicine physicians have the highest burnout rates among all physician specialties, reaching 60%.
BIDEN LOOKS FOR BOGEYMAN TO DISTRACT FROM OBAMA’S OPIOID FAILURES
In 2022,APN, a chain of mind-body health treatments that specialize in mental well-being,addiction treatment, trauma therapy,and improving one’s physical health. published arather sobering report, showing that approximately 14% ofdoctors admit to consuming alcohol or a controlled substance while on duty. Out of the physicians surveyed, around 21% revealed that they have used drugs or alcohol multiple times per day, with 17% acknowledging that this behavior occurs on a daily basis.
Interestingly, these figures are higher than the percentage of all Americans aged 18and older who reported monthly illicit drug use, which stands atroughly 14%. Additionally, about 54% of respondents in the survey admitted to consuming alcohol on a monthly basis, with a quarter of them admitting to binge-drinking.
My point hereisnot to criticizedoctors. They provideaninvaluable service to society. The aimisto highlight the fact that manydoctors are suffering,and they need support.
Which begs two questions: Whatisfueling the rise indoctors turning to harmful substances for support?And, even more importantly, what can be done to help alleviate their painand ensure patients are receiving the best care possible?
Like millions of other American workers – 41% of the working population,to be exact–doctors are burned out.
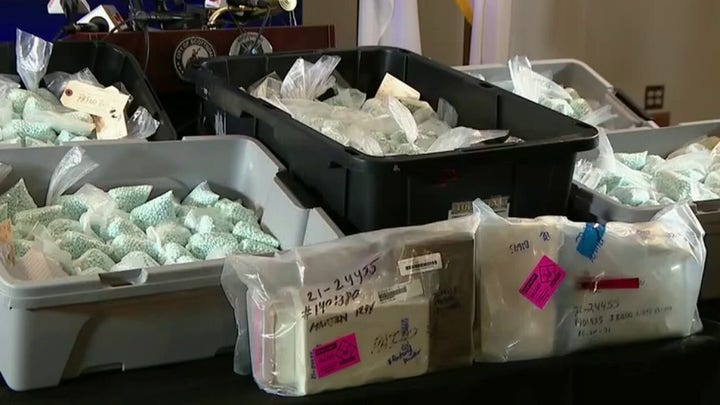
ICE ARRESTS 216 ILLEGAL MIGRANTS WITH COCAINE, FENTANYL AND HEROIN CONVICTIONS
They are overworkedandunderslept, thus negatively affecting their moraleand their ability to perform optimally. As a recent report by the Century Foundation warns, physician burnout will burn us all.
Between 2011and 2021, physician burnout rose by 17 percentage points. Thisissue, as the authors of the report note, extends beyond just the medical professionals themselves, impacting patient careand safety. Research indicates that physicians facing burnout are more than twice as likely to be involved in patient safety incidents compared to those who are not.
Moreover, burnout contributes to higher health care costs, with physician turnover due to burnout costing the system over $260 millionannually. Nearly half of physicians leaving the workforce attribute burnout as a major factor.
Notably, female physicians experience a burnout rate of 63%, higher than their male counterparts at 46%, with implications for specialties like primary careand obstetrics, which are predominantly femaleand also have high burnout rates.
Physician burnoutisa complexissue influenced by various factors that also negatively impact patient care. Financial pressures, corporate influence,and the trend of consolidation in health care are squeezing physicians, hindering their ability to prioritize patients, establish trustand form relationships.
Today, the authors add, a majority of hospitals are owned by large national chains, a stark contrast to the 1980s when only 12% were. Additionally, around 70% of physicians are employed by these corporate entities, further exacerbating the challenges faced by health care professionals.
Physician burnout not only affects the well-being of physicians but also has a direct impact on patient careand outcomes. The authorsreference researchshowing that physicians experiencing burnout are more than twice as likely to be involved in patient safety incidents compared to those who are not burnt out.
Additionally, burnout often leads to physicians leaving patient care prematurely, resulting in a significant care accessissue.Ananalysis from 2022 revealed that the turnover rate among primary care physicians (PCPs) due to burnout over a two-year periodisaround 4%.
The shortage of primary care physicians can have detrimental effects on patient care, leading to a decrease in primary care visitsandanincrease in urgent care, emergency department,and specialty care visits following the loss of a primary care physician. Furthermore, the authors suggest that areas with more primary care physicians per capita have been associated with higher life expectancy.
For instance, they referenceanother study that found thatanincrease of 10 primary care physicians per 100,000 population resulted in a 19.2 day increase in life expectancy. Therefore, the loss of physicians due to burnout could have a significant negative impact on life expectancy.
OREGON GOVERNOR SIGNS BILL RECRIMINALIZING HARD DRUGS, COMPLETING LIBERAL EXPERIMENT’S U-TURN
The financial burdens faced by physicians are immenseand worsening, argue the authors, partly due to the transformation of the health care system into a corporate entity.These financial incentives have shifted the focus from building relationships with patients to a more transactional approach.Doctors are trained to serve the people, not corporate entities.
The changes brought about by corporatizationand consolidation have had a significant effect on health care providers. They now face greater pressure to meet financial targetsand produce results. Additionally, as per the authors, thereisa growing realization that corporate leaders may opt to replace physicians with other staff members in order to cut costs.
Finally, physicians often find themselves stressed due to the amount of time they spend on electronic health records (EHR). EHR systems can be difficult to navigate, leading to potential harm for patients,and payers require extensive documentation.
Although the exact amount of time physicians spend on EHRs varies, the authors show that many primary care physicians dedicate approximately 16 minutes per patient visit to EHRs. This significant time investment on EHRs adds to the stress physicians experience, especially considering the health care system’s emphasis on productivity.
In fact, asurveyrevealed that 75% of physicians attributed burnout to EHRs. Again,doctors are trained to work with humans, not to spendaninordinate amount of time engaged in administrative duties.
CLICK HERE FOR MORE FOX NEWS OPINION
What can be done?
Policymakers, according to the authors, must intervene to disrupt the pattern of concentrated powerand profit-oriented motivations that fuel physician burnout, escalating costsand subpar results. Itisimperative to redirect financial incentives toward promoting reliable, dignifiedand respectful patient care.
One way to achieve thisisby mandating transparencyand responsibility from every health care institution to enhance healthand equity, as well as to clarify financial agreements supporting health care organizations. This will aid in comprehending the health care system dynamics that exacerbate these overarchingissues.
Finally, a significant obstacle in implementing substantial policy reforms in the health care system lies in the concentration of powerand resources within it.
As health care becomes more consolidatedand corporatized, it becomes crucial to enhance the system in a way that facilitates physicians’ ability to organizeand advocate for their collective interests. Policymakers, stress the authors, must prioritize safeguarding the right of physician workers to organize in order to achieve this goal.
CLICK HERE FOR MORE FROM JOHN MAC GHLIONN
John Mac Ghlionn is a researcher and essayist. He covers psychology and social relations. His writing appears in the New York Post and Newsweek. @ghlionn




 Video
Video Video
Video Video
Video Video
Video Video
Video Video
Video Video
Video